Investigation Pathway
Fellows on the Investigation Pathway aim to pursue careers as physician investigators, advancing the field of nephrology through research, from Basic Science, to Translational and Clinical Science. Some fellows on the Investigation Pathway enter the program with an area of research or even a project in mind while others identify their research focus from a formative clinical experience during the first year. By winter of the first year, fellows have had ample opportunity to meet with faculty to discuss their interests and choose a mentor whose scientific and career guidance will help them launch their promising academic career.
During their second and third years, fellows on the Investigation Pathway conduct original research under the mentorship of a faculty member at BWH, MGH or one of our affiliated institutes. As part of the research years, fellows participate in didactics and other formal opportunities to learn research techniques and methods and develop the skills they will need for success as an investigator. Fellows are expected to write grants early in the second year, a valuable experience that requires them to develop expertise in their area of investigation, construct the case for their project’s scientific merit, and learn the art of grant writing and grantsmanship under the tutelage of their scientific mentor. Fellow research years are supported by a combination of institutional grants and funds as well as individual fellowship grants to fellows. Our fellows have been remarkably successful in obtaining individual fellowship grants from the NIH (F32), the VA, from foundations such as the American Society of Nephrology, American Heart Association, American Kidney Fund and American Society of Transplantation, and from industry. During their research years, fellows are supported to attend ASN Kidney Week, an invaluable opportunity to learn from their peers and others in their chosen space, network, and of course compete in the FIT Bowl!
Fourth Year
An optional fourth year of fellowship training is available depending on the fellow’s interests, training needs, and career goals. Fourth year of fellowship can include additional clinical training (for example, transplant or interventional nephrology fellowship) or allow more time to publish their work and enhance their candidacy for, and write, a career development grant. Fourth year of training is funded through an individual fellowship grant (e.g. NIH-F32, AKF, ASN, AHA, AST) or through bridge funding provided by the respective renal division where the fellow will be joining the faculty. Many fellows extend their fellowship time beyond 3 years to pursue additional training or devote more time to research in preparation for joining our faculty or the faculty of other medical schools.
Areas of Investigation
Basic and Translational Science
Opportunities for basic and translational science research abound. Fellows can choose to work with faculty at either the BWH or MGH renal divisions or with affiliated institutions such as Children’s Hospital Boston, the Broad Institute, the Wyss Institute for Biologically Inspired Engineering, the MIT Institute for Medical Engineering and Science, as well as faculty throughout Harvard and MIT. Fellows pursuing basic or translational science participate in division-sponsored summer programs to learn the techniques employed in basic and translational research such as ELISA, Western Blot, PCR, and working with animals. They also often attend the Models of Disease Boot Camp sponsored by the Harvard Catalyst geared toward fellows embarking on their basic and translational science research years and the Mount Desert Island Biological Laboratory Origins of Renal Physiology Course. Fellows also attend and present at division basic science research conferences, learning from other investigators and benefiting from the peer mentorship and support of other trainees.
Research Areas
Jodie Babitt
Endothelial cell biology in hepatorenal syndrome
Joseph Bonventre
Mechanisms of AKI and AKI to CKD transition with discovery of new therapeutics
Creation of kidney cell populations to create a wearable artificial kidney
M. Amin Arnaout
Role of integrins in ischemia-reperfusion injury models
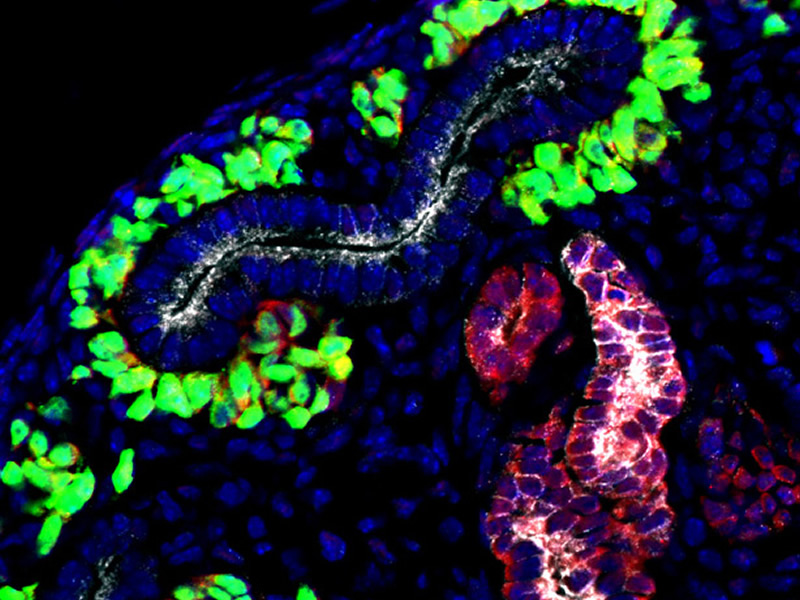
Ryuji Morizane
Recreating Kidney Organogenesis in vitro with Human Pluripotent Stem Cells
Jamil Azzi
Development of liquid biopsy for patients with kidney disease using urinary exosomes
Joseph Bonventre
Core Laboratory to measure biomarkers of kidney function and injury
Eugene Rhee
Metabolomic and proteomic markers of kidney disease
Leonardo Riella
Point-of-Care urine assay using CRISPR/cas13 to monitor transplant patients
Venkata Sabbisetti
Discovery and validation of biomarkers using omic technologies, identification of novel therapeutic targets in kidney disease
Ryuji Morizane
Vascularized kidney organoids on chip for efficacy and toxicity testing of somatic genome editing
M. Amin Arnaout
Development of microfluidic devices for dialysis
Joseph Bonventre
Microphysiological systems incorporating human kidney cells generated from stem cells
Luke Lee
Kidney Microphysiological Analysis Platforms (MAP) to Optimize Function and Model Disease
Ryuji Morizane
Biomanufacturing of Vascularized Kidney Tissues: A Foundational Step towards Building a Kidney
M. Amin Arnaout
Mechanisms of cyst formation in Autosomal Dominant Polycystic Kidney Disease
Peter Czarnecki
Biochemical mechanisms of intracellular signal transduction that give rise to PKD/other cystic genetic disease
Anna Greka
Genetics and genomics of kidney diseases
Ryuji Morizane
CRISPR/Cas9-based Targeted Genome Editing for the Development of Monogenic Diseases Models with Human Pluripotent Stem Cells.
David Mount
Translational genomics of hyperuricemia
Matt Sampson
Kidney disease genomic discovery using population-based, multiomics strategies
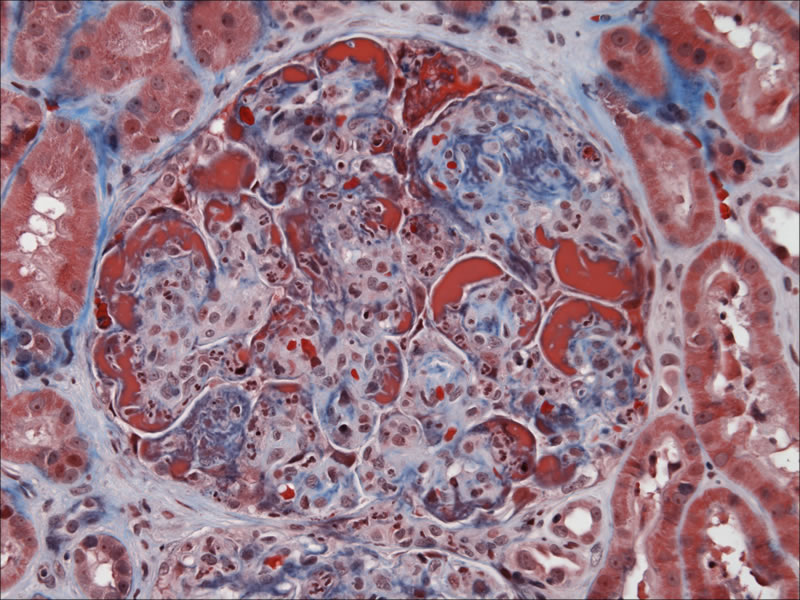
Autoimmune Renal Disease
Anna Greka
Podocyte biology and targeted therapeutics
Vicki Kelley
Innate and adaptive immune mechanisms driving inflammation
Angela Schmider
Studying the assembly and architecture of the leukotriene synthetic complex in myeloid cells
Roy Soberman
Signal integration and macromolecular organization in cells of the immune system
Transplant
M. Amin Arnaout
Role of integrins in delayed graft function
Jamil Azzi
Toward targeted therapies in auto and allo-immunity: Immune regulation and beyond
Leonardo Riella
Mechanisms and Targets of Immune Regulation in Transplantation: from Bench to Bedside
Peter Sage
Cellular Immunology of Antibody Mediated Diseases
Joseph Bonventre
Study of the effects of AKI on the development and progression of kidney fibrosis
Li-Li Hsiao
Mechanisms of CKD-related cardiovascular complications especially distant tissue fibrosis
Ryuji Morizane
Modeling Kidney Fibrosis in Kidney Organoids derived from Human Pluripotent Stem Cells
Sahir Kalim
Protein and metabolite alterations in uremia
Eugene Rhee
Kidney metabolism in health and disease
Sylvie Breton
Regulation of epithelial cells in the urogenital tract
Dennis Brown
Vasopressin action – intracellular trafficking pathways of aquaporin 2 water channels
Susan Cheung
Signaling pathways modulating aquaporin 2 trafficking and expression affecting water balance disorder
Mahmoud Nasr
Studying the initial events that lead to viral infection at the molecular level
Jodie Babitt
Crosstalk between iron, anemia, inflammation and CKD-MBD
Harald Jueppner
Calcium and phosphate regulation
Petra Simic
Kidney-bone interaction
M. Amin Arnaout
Structure and function of integrins in the kidney
Mahmoud Nasr
Heterotrimeric G protein signaling in kidney diseases
Johannes Van Agthoven
Structural biology and antagonist design of Integrin
Clinical Science and Epidemiology
Nearly every possible area of clinical research is represented across our institutions, with opportunities to work with mentors at BWH, MGH, the VA, Harvard TH Chan School of Public Health (HSPH), data scientists at MIT, and beyond. Fellows pursuing clinical science learn biostatistics and epidemiologic methods and other skills required to pursue clinical research. In addition to regular meetings with their mentor, fellows participate in laboratory meetings and division clinical research conferences where they present their work and learn from faculty and peers in a collaborative and supportive environment.
Research Areas
Andrew Allegretti
Hepatorenal Syndrome, AKI in cirrhosis
Joseph Bonventre
Mechanisms of AKI and AKI to CKD transition with discovery of new therapeutics
Kenneth Christopher
Critical Care Metabolomics
Peter Czarnecki
CRRT and volume management in critical illness, COVID and AKI
Shruti Gupta
Outcomes of COVID-19 in critically ill patients
David Leaf
Identifying novel risk factors and mechanisms of AKI, and therapies for its prevention and treatment
Mallika Mendu
Implementation of a standarized algorithim related to RRT initiation and catheter placement (AKI SCAMP)
Anemia and Iron in CKD
Finnian McCausland
Trajectory of hemoglobin changes during CKD, risk factors for anemia, and the association of hemoglobin with outcomes
Ajay Singh
Development of new anemia treatments in patients with kidney disease
Cardiovascular Disease in CKD
Finnian McCausland
Cardio-renal interactions and risk factors for heart failure and CKD progression – observational studies and interventional trials
Dialysis
Sahir Kalim
Protein carbamylation, amino acid balance, and uremic toxins in CKD
Finnian McCausland
Modifiable risk factors for intra-dialytic hypotension and cardiovascular disease in hemodiaysis – observational studies and interventional trials
Geriatric Nephrology and Palliative Care
Sahir Kalim
Chronic pain and opioid use in ESRD patients
Ernest Mandel
Serious Illness Communication in Advanced CKD and ESRD
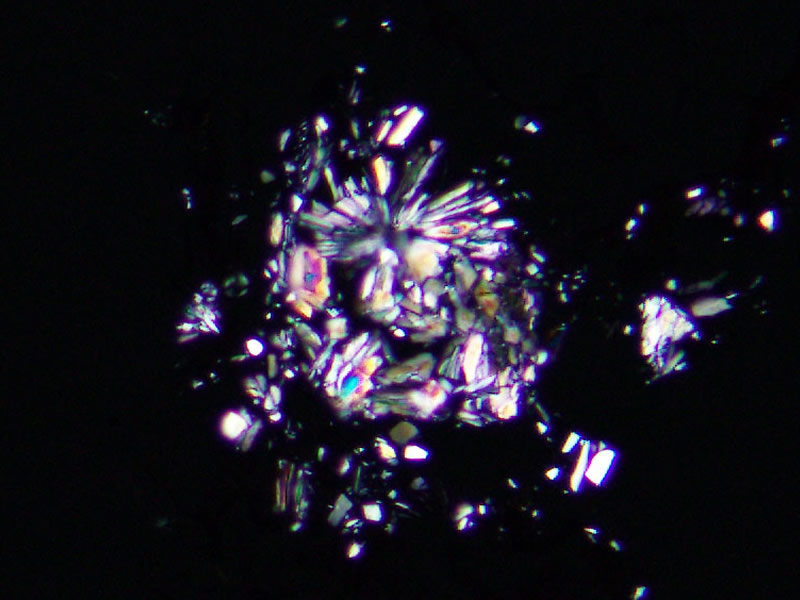
Mineral Bone Disease
Sagar Nigwekar
Risk factors, pathogenesis, and treatment of calcific uremic arteriolopathy (calciphylaxis)
Nutrition in CKD
Lea Borgi
Nutrition and Chronic diseases
Kenneth Christopher
Nutritional metabolomics
Sahir Kalim
Protein carbamylation and amino acid therapy in ESRD
Pharmacoepidemiology
Julie Paik
Comparative effectiveness, safety monitoring, prescribing
Infection Prevention and Management
Gary Curhan
Risk factors for infections requiring hospitalization in patients with CKD
Anil Chandraker
Clinical trials in transplantation
Anna Greka
Abatacept in Treatment Resistant Nephrotic Syndrome
Gearoid McMahon
ASCEND: Trial of prolyl hydroxylase inhibitors in patients with CKD and ESRD
John Niles
Avacopan in C3GN; MAINTANCAVAS: Maintenance treatment in ANCA vasculitis
Nina Tolkoff-Rubin
Eculizumab for recurrent aHUS post transplant
Leonardo Riella
Novel drug targets and dietary interventions to promote immune regulation in humans
Meghan Sise
Clinical trials in Hepatitis C virus infection and HCV+ to HCV-naive kidney transplantation
Ethics in Nephrology
Valerie Luyckx
Ethics of ESRD care
Ernest Mandel
Resource allocation in AKI and ESRD care
Global Health in Nephrology
Valerie Luyckx
Kidney disease management in low- and middle-income countries
Mohammed Sayegh
Conflict and disaster nephrology: ESRD care in refugee and other stressed populations
Population Health Management
Li-Li Hsiao
Community outreach and education programs (KDSAP)
Mallika Mendu
Development of network-wide CKD registry, population health-based innovations to improve care delivery
Quality and Safety
Mallika Mendu
Care delivery innovation research to improve quality and safety for kidney disease patients
Gary Curhan
Risk factors and multi-omics approach to prevention of kidney stones
Julie Paik
Risk factors for fractures
Academic Clinician-Educator (ACE) Pathway
The Academic Clinician-Educator (ACE) Pathway aims to prepare fellows to assume leadership roles in academic medical centers as clinical experts and medical educators. In addition to 8 weeks of inpatient rotations at BWH or MGH, ACE Pathway fellows identify an area of clinical expertise in which they wish to gain more specialized experience while simultaneously pursuing scholarly activity to build their academic portfolio. Scholarly activity can include writing chapters and reviews, conducting clinical research within their identified area of clinical expertise, or pursuing medical education scholarship, from curriculum development to medical education research. ACE Pathway fellows have ample opportunities to develop and hone their teaching skills, including formal teaching of medical students and residents, attending opportunities on teaching services alongside dedicated academic clinician-educator faculty, and in formal didactics offered by Centers of Excellence at both institutions as well as the Harvard Macy Institute.
Areas of Clinical Expertise
Clinical Training:
- Gain additional experience on our Renal ICU services
- Rotate in medical and surgical ICUs to gain further exposure to ICU medicine, ventilator management, cardiac devices and technologies including tailored therapy, VAD, ECMO
- Hone temporary access placement skills and develop other skills such as ultrasonography and POCUS
- Attend ASN Critical Care Nephrology Early Program with divisional support
- Pursue formal fellowship training in Critical Care Medicine
Scholarly Opportunities:
- Participate in clinical trials of AKI prevention or treatment including CRRT
- Study ICU outcomes using clinical epidemiology and data science approaches
- Engage in a quality and safety project around issues of concern in critical care nephrology
Clinical Training:
- Gain broad exposure to geriatrics in a dedicated, multidisciplinary geriatric nephrology clinic at the VA
- Rotate at Hebrew SeniorLife, the geriatrics arm of Harvard Medical School, with a robust geriatric dialysis program
- Develop specialized experience in renal palliative care by rotating with the Kidney Pal program, a dedicated renal palliative care service at BWH in the inpatient and outpatient setting
- Build strong foundation of palliative care knowledge and skills through the Harvard Center for Palliative Care’s Practical Aspects of Palliative Care (PAPC) Program
- Pursue additional formal fellowship training in either Geriatrics or Palliative Care
Scholarly Opportunities:
- Complete an education-focused project as part of the Harvard Center for Palliative Care’s Palliative Care Education and Practice (PCEP) Program
- Participate in active clinical research in geriatric nephrology or renal palliative care at BWH, MGH, or the VA
Clinical Training:
- Attend dialysis access clinics to hone access evaluation and examination skills
- Observe access procedures such as arteriovenous fistulograms, angioplasties, stent placements, and thrombectomies with interventional nephrologists and radiologists
- Scrub in to access creation surgeries
- Gain additional experience in temporary dialysis catheter placement
- Perform native and transplant kidney biopsies under ultrasound guidance
- Receive formal training in ultrasonography, including renal ultrasonography and Point of Care Ultrasound for evaluation of volume status
- Pursue formal interventional nephrology training through ASDIN-accredited programs at both BWH and MGH
Scholarly Opportunities:
- Engage in quality and safety projects on dialysis access
- Conduct clinical research on the use of POCUS in nephrology
- Develop and design educational curricula in access examination or POCUS
Clinical Training:
- See patients in dedicated onco-nephrology clinics at the Dana Farber Cancer Institute and MGH Cancer Center
- Rotate with onco-nephrology faculty on the dedicated DFCI/BWH oncology service
- Attend ASN Onco-Nephrology Early Program with divisional support
Scholarly Opportunities:
- Identify and describe renal sequelae of emerging cancer therapies
- Pursue clinical research into AKI and glomerulopathies in stem cell transplantation
- Explore the application of oncologic therapies, such as CAR-T cells, to renal disease
Clinical Training:
- Care longitudinally for a shift of in-center hemodialysis patients
- Gain advanced knowledge in home modalities such as home hemodialysis and peritoneal dialysis through dedicated experiences
- Elective rotations with interventional nephrology for further experience with dialysis access assessment and management
- Pair with faculty medical directors for exposure to dialysis medical directorship and quality programs
- Attend dialysis Medical Director meetings, Home Dialysis University, or Nephrology Business Leadership Program with divisional support
Scholarly Opportunities:
- Engage in quality and safety projects in dialysis
- Pursue a clinical research project in dialysis
- Develop educational curricula or assessment tools for dialysis education
Clinical Training:
- Care for transplant patients through transplant continuity clinic
- Participate in donor evaluation clinics
- Observe living and deceased donor surgeries and gain experience in organ procurement
- Rotate through tissue typing and histocompatibility laboratories
- Perform transplant biopsies under ultrasound guidance and review pathology findings with world-renowned pathologists
- Rotate through vasculitis and glomerulonephritis clinics to gain further experience with immunosuppression management
- Pursue formal transplant fellowship through AST-accredited transplant nephrology fellowships at both BWH and MGH
Scholarly Opportunities:
- Participate in a wide range of clinical research projects in transplantation
- Teach and develop curricula for teaching immunology and transplant medicine
Clinical Training:
- Rotate through clinics at the MGH Vasculitis and Glomerulonephritis Center (VGN), a world-renowned ANCA and anti-GBM referral center, and the BWH glomerular diseases clinic
- Care for patients in clinics specializing in infection-related glomerulonephritis at MGH
- Gain exposure to laboratory assays and enhance native kidney biopsy experience
- Review pathology findings with world-renowned pathologists
- Attend the ASN Kidney Week Early Program in Glomerular Diseases with divisional support
Scholarly opportunities:
- Participate in clinical research trials and outcomes studies at the VGN
- Study novel experimental therapeutics for glomerular disease at the BWH Glom-NExT Center